Permedion
Permedion is a wholly owned subsidiary of Gainwell. Permedion provides utilization management services to help safeguard against unnecessary or inappropriate use of services and against excess payments. Services include prior authorization, prepayment and post-payment clinical reviews to help ensure that inpatient and outpatient services are medically necessary, occur in the appropriate setting, are billed appropriately and are of the highest quality.
We also provide Independent Review Organization services for state Departments of Insurance and other entities under the Patient Protection and Affordable Care Act to evaluate Medical Necessity and Experimental/Investigational appeals and review Quality of Care issues for state licensing agencies.
Permedion is designated by the Centers for Medicare & Medicaid Services (CMS) as a Quality Improvement Organization (QIO)–like entity and accredited by URAC for both Health Utilization Management and Independent External Review.
For additional information about Permedion please contact .
Massachusetts Medicaid
MassHealth Acute Hospital Utilization Management Program
Permedion performs utilization management services on behalf of the Executive Office of Health and Human Services, to ensure medical and surgical services provided to members are medically necessary, are delivered in the most appropriate and cost-effective setting, billing is compliant and that members receive the quality of care that is consistent with professionally recognized standards. Components of the utilization management program include the retrospective review of prepayment and post-payment claims as well as pre-admission screening for all elective inpatient hospital admissions. For inquiries related to this contract, please email .
New Jersey Medicaid
NJ FamilyCare Utilization Review Audits
Permedion provides utilization review services on behalf of the New Jersey Department of Human Services, Division of Medical Assistance and Health Services. The scope includes clinical audits of acute care general hospitals, private psychiatric hospitals, comprehensive rehabilitative hospitals and specialty hospitals for both fee-for-service and managed care claims.
For inquiries regarding this contract please email .
Ohio Medicaid
Fee For Service Hospital Utilization Management Program
Permedion supports the Ohio Department of Medicaid’s statewide clinical utilization management and prior authorization program for hospital and other services provided to Ohio Medicaid consumers.
For questions regarding Fee for Service Prior Authorization / Precertification requests, retrospective review or other general questions please email .
Ohio Managed Care Entity External Medical Review
Providers who disagree with the Ohio Medicaid Managed Care Entity’s determination on appeal to deny, limit, reduce, suspend, or terminate a covered service for lack of medical necessity may request an External Medical Review with Permedion. The request for External Medical Review must be submitted to Permedion within 30 calendar days of the written notification that the internal appeals process has been exhausted. Providers may also request an External Medical Review if the MCE has not met the required Provider Internal Appeal or Provider Claim Dispute resolution time frame for a denial based on medical necessity.
Providers must complete the Ohio Medicaid MCE External Review Request form and submit to Permedion together with the required supporting documentation. Upload this request form and supporting documentation to Permedion’s provider portal (new users will send their documentation through secured email at to establish portal access). Providers should attach to this request form only additional documents not originally provided to the MCE during their review process.
For more information about the External Medical Review process, please contact Permedion at 1-800-473-0802, Option 2.
Forms:
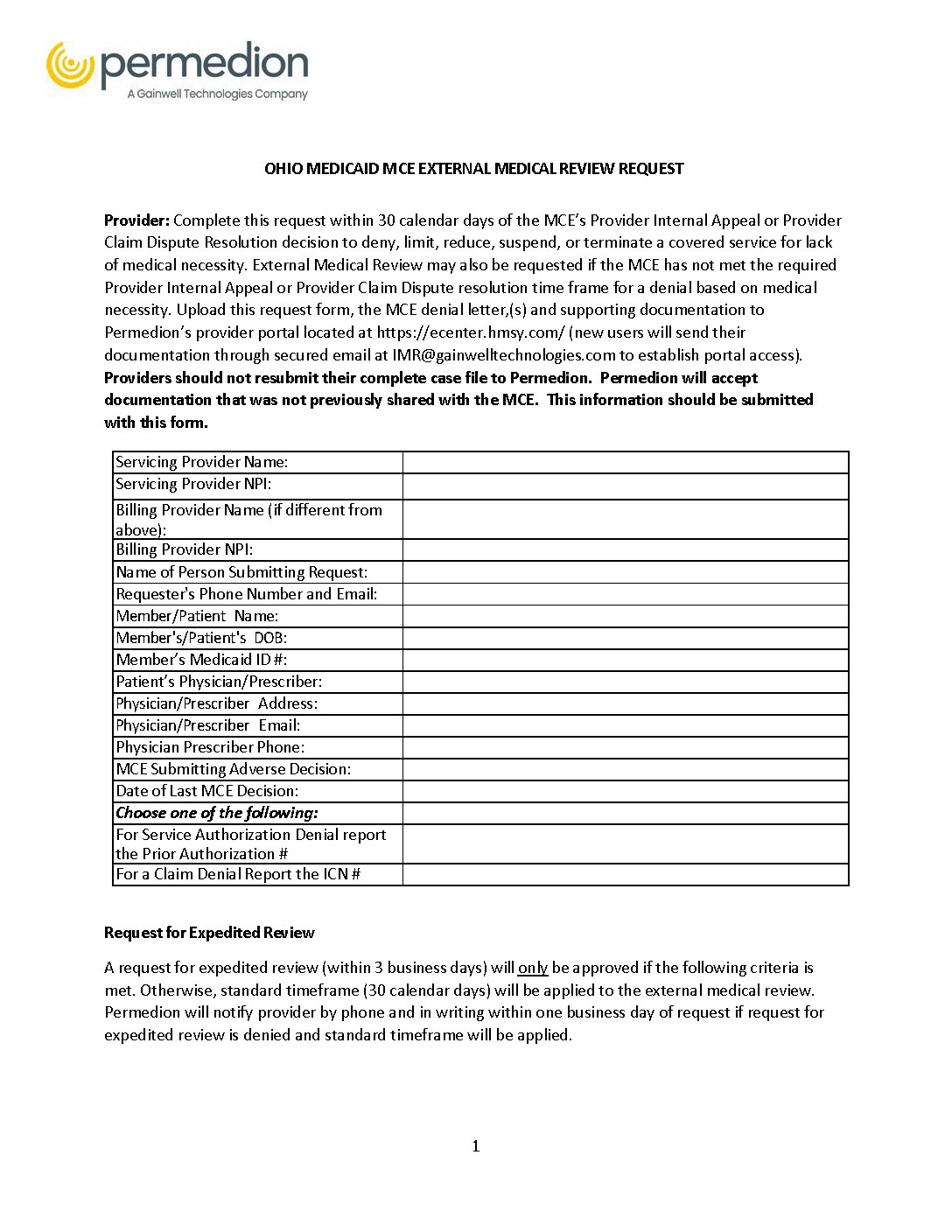
Ohio Medicaid MCE External Review Request
Download PDF
3 pages; 194 KB

Ohio Medicaid HomeHealth PriorAuthorization Request Form
Download PDF
3 pages; 246 KB

Ohio Medicaid Inpatient Psychiatric Precertification Request Form
Download PDF
5 pages; 312 KB

Ohio Medicaid Permedion Portal Quick Reference Guide
Download PDF
14 pages; 1 MB
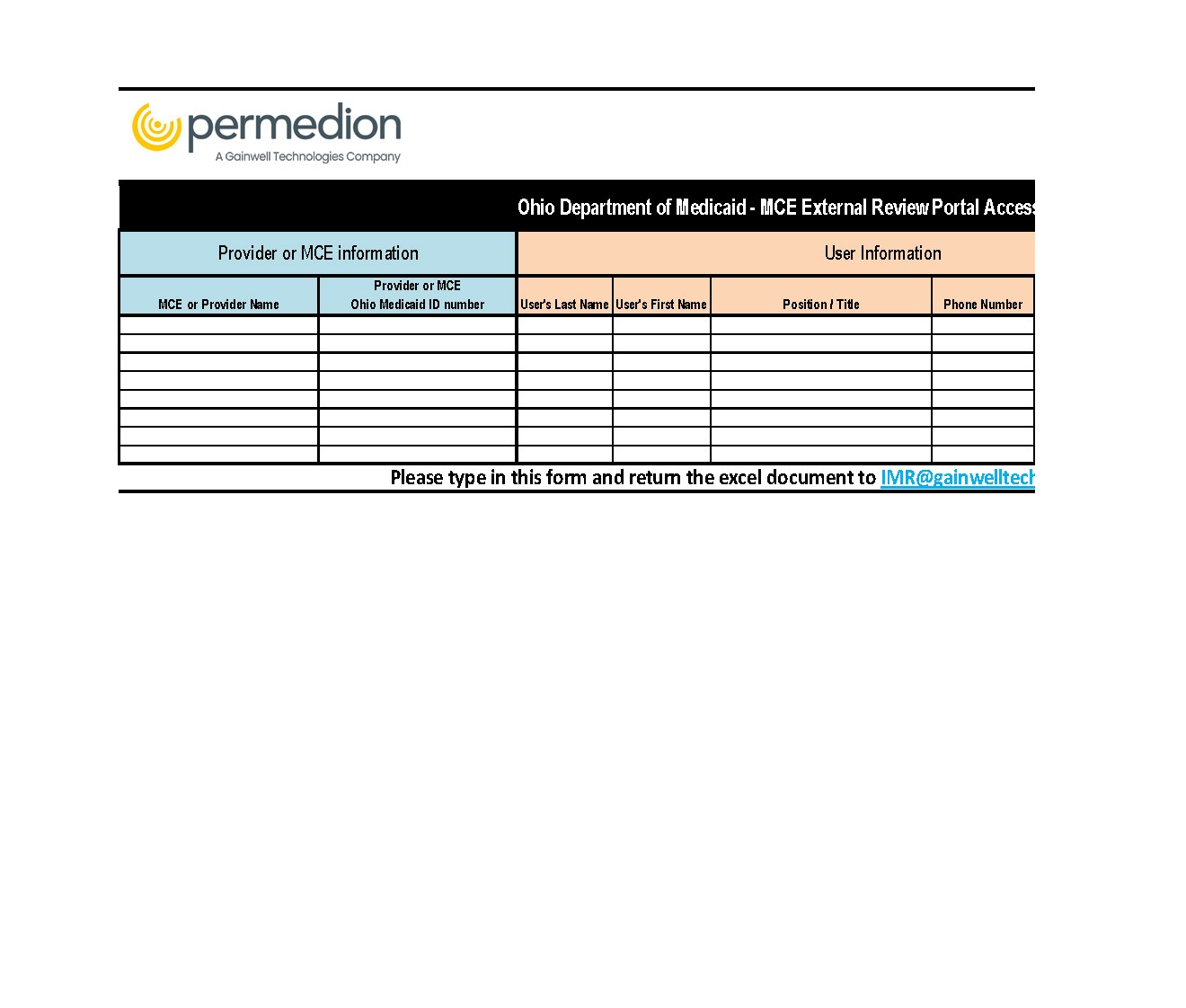
Portal Access Request Form
Download Excel File
44 KB

